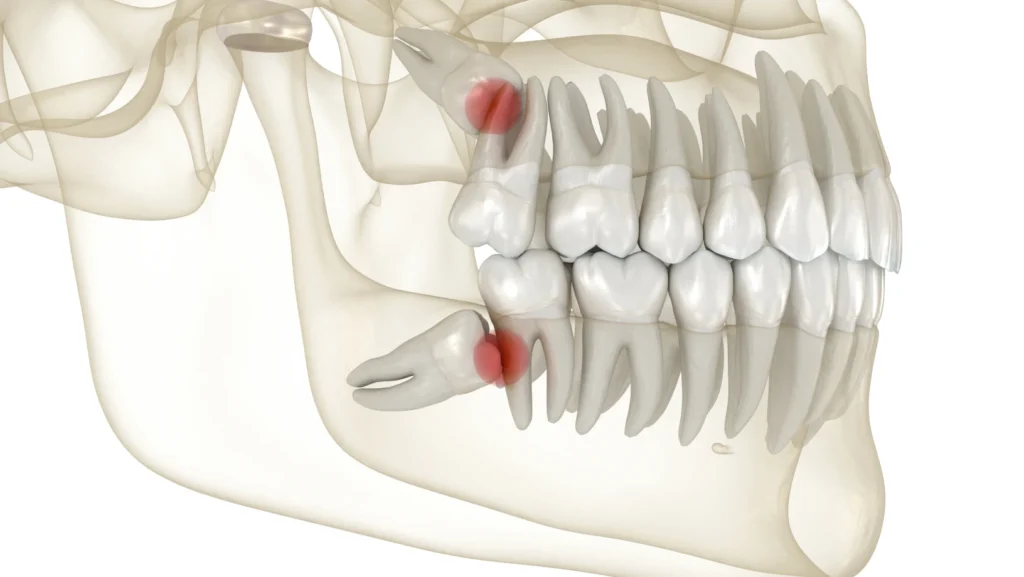
Wisdom teeth, also known as the third molars, are the teeth at the back of your mouth. They are usually the last adult teeth to erupt (between 17 and 21 years of age).
Wisdom teeth are often removed due to one or more of the following reasons:
- Lack of space in the back of the mouth to allow straight eruption.
- Orthodontic reasons.
- Persistent and/or recurrent pain and/or infection.
- Development of tooth decay, bone cyst.
- Possible damage to the adjacent teeth (decay or gum disease).
- Prophylactic (or preventative) removal (difficulty cleaning due to their position and/or orientation).
Description of the procedure
The procedure is performed under local anaesthetic in our surgical suite under optimal aseptic conditions.
Sedation (optional):
If you are nervous, you may be given a sedative medicine to help control any anxiety.
Blood sampling and PRF production:
On the day of the operation, a blood sample is generally taken from the crease of the elbow to produce the PRF by recovering your blood’s white blood cells and platelets (cells involved in immune defenses and wound healing).
The procedure:
The gum may be reflected from the jaw bone surface and teeth are carefully removed. Occasionally the surgeon may need to remove some bone surrounding the wisdom tooth. The extraction sites are then cleansed and an absorbable collagen or PRF material is directly applied to accelerate the healing process and decrease postoperative bleeding and infection. Absorbable sutures will dissolve in 2 weeks.
What is PRF?
Platelet-rich fibrin (PRF) is a mixture of white blood cells, fibrin, platelets, stem cells and growth factors. PRF is made by drawing a small amount of blood and spinning it in a centrifuge.
There are no blood additives or chemicals. Only extracts from the patient’s own blood drawn just before the surgical procedure.
The PRF gets applied directly to areas that require healing, such as cavitation left behind from an extracted tooth. It possesses amazing natural healing properties.
PRF not only speeds the healing process, but it decreases postoperative inflammation/pain and infections and avoids having dry sockets when the clot does not form naturally or properly.
Coronectomy and leaving root fragments behind :
Occasionally if the roots are very deep, curled or wrapped around the lower jaw nerves, it may be decided to perform a “Coronectomy”.
Which means to remove most of the tooth, leaving behind some of the root intentionally to avoid any nerve injury.
If a fragment of the root is left behind, the majority of the time it will heal very well with no complication. The root will remain deep or may ‘float’ up to the top of the gum, where it is more easily and safely removed at a later stage (between a few months – years).
Also learn about : Exposure of impacted teeth
What is an impacted (unerupted) tooth?
An impacted (unerupted) tooth is a tooth that fails to fully pass through the gum tissues as something (dense soft tissue, bone, tooth malposition, cysts, or another tooth) prevents its normal eruption into the mouth. If a tooth fails to emerge, or emerges only partially, it is considered to be impacted. The patient is usually referred by his/her Orthodontist.
Patients frequently develop problems associated with impacted wisdom teeth, which are the most common form of impacted teeth that need removal. The second most common teeth to become impacted are the maxillary cuspids (canine). Other commonly impacted teeth include the second molars, bicuspids, and the lower jaw cuspids.
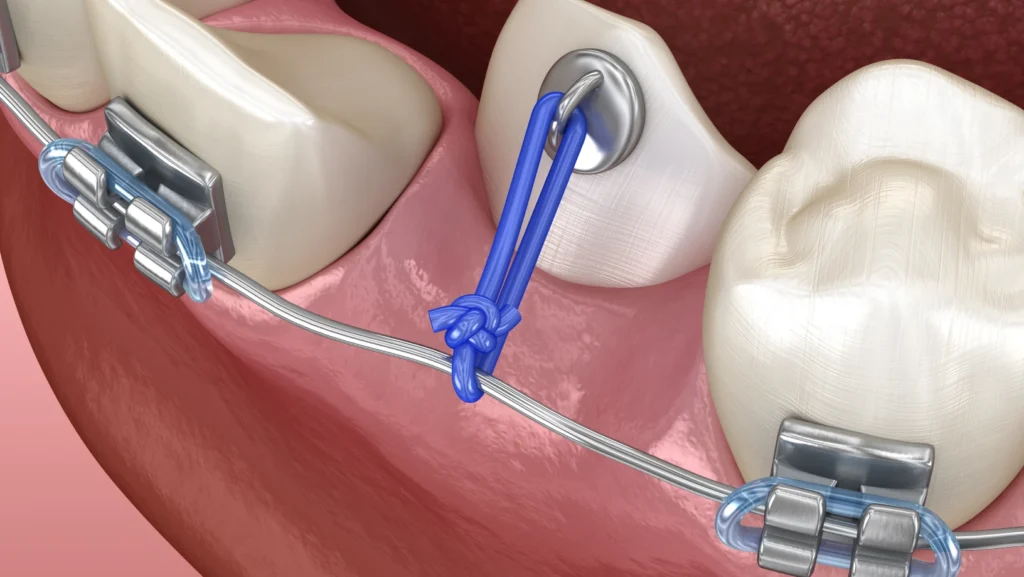

Exposure of the unerupted tooth
Frequently, the primary tooth or the supernumerary tooth that is blocking the eruption of the impacted tooth is removed during the procedure.
Once the tooth is exposed, an orthodontic bracket and chain is bonded to it. The chain will then be attached to the orthodontic appliance (previously placed by your orthodontist) where it will remain temporarily.
Following healing, you will be referred back to your orthodontist where he/she will slowly move the exposed tooth into its proper position in the dental arch.
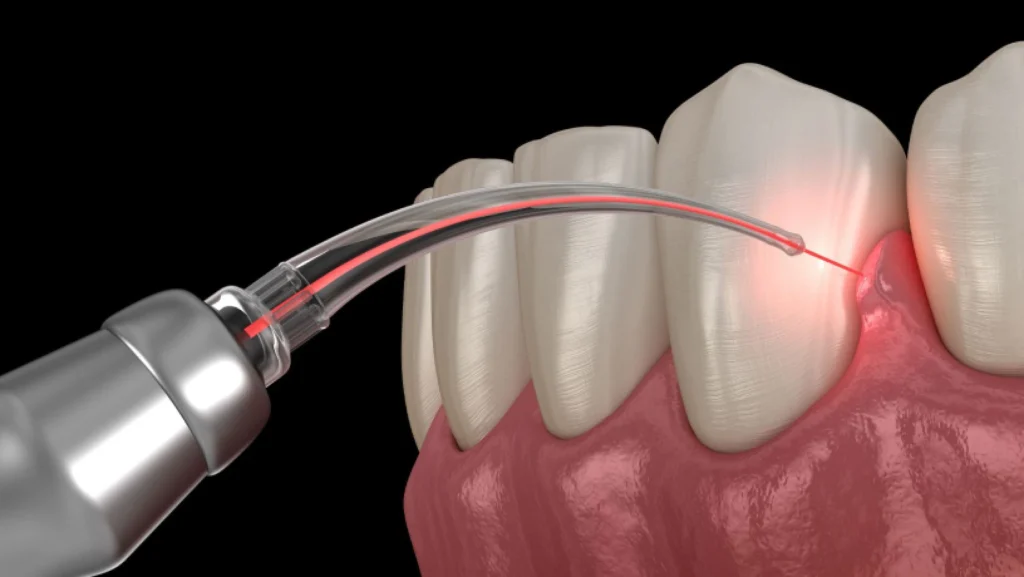
Also learn about : Frenectomy
Labial frenectomy
Labial frenectomy – is a surgical technique that aims to remove the frenulum with its attachment. Frenectomy, is indicated if the frenulum attachment is close to the teeth and causes midline diastema (gap), gingival recession, hindrance in maintaining adequate oral hygiene, or if it interferes with orthodontic or prosthetic needs.
Lingual frenectomy
Lingual frenectomy – is indicated when the frenulum that attaches the tongue to the floor of the mouth is shorter than usual and causes ankyloglossia (tongue-tie).
Ankyloglossia is a very common congenital anomaly that affects both children and adults. A frenulum that is too short restricts the mobility of the tongue to varying degrees and can cause a speech impediment or limit the growth of the mandible.
Description of the procedure
If you are nervous, you may be given a sedative medicine to help control any anxiety. After local anesthetics have numbed the area, the frenulum is removed. Absorbable sutures will dissolve in 2 weeks.
Rehabilitation with a speech therapist is generally recommended after removal of the tongue tie.
Also learn about : Periodontal surgery